Diabetes Management Kumbakonam
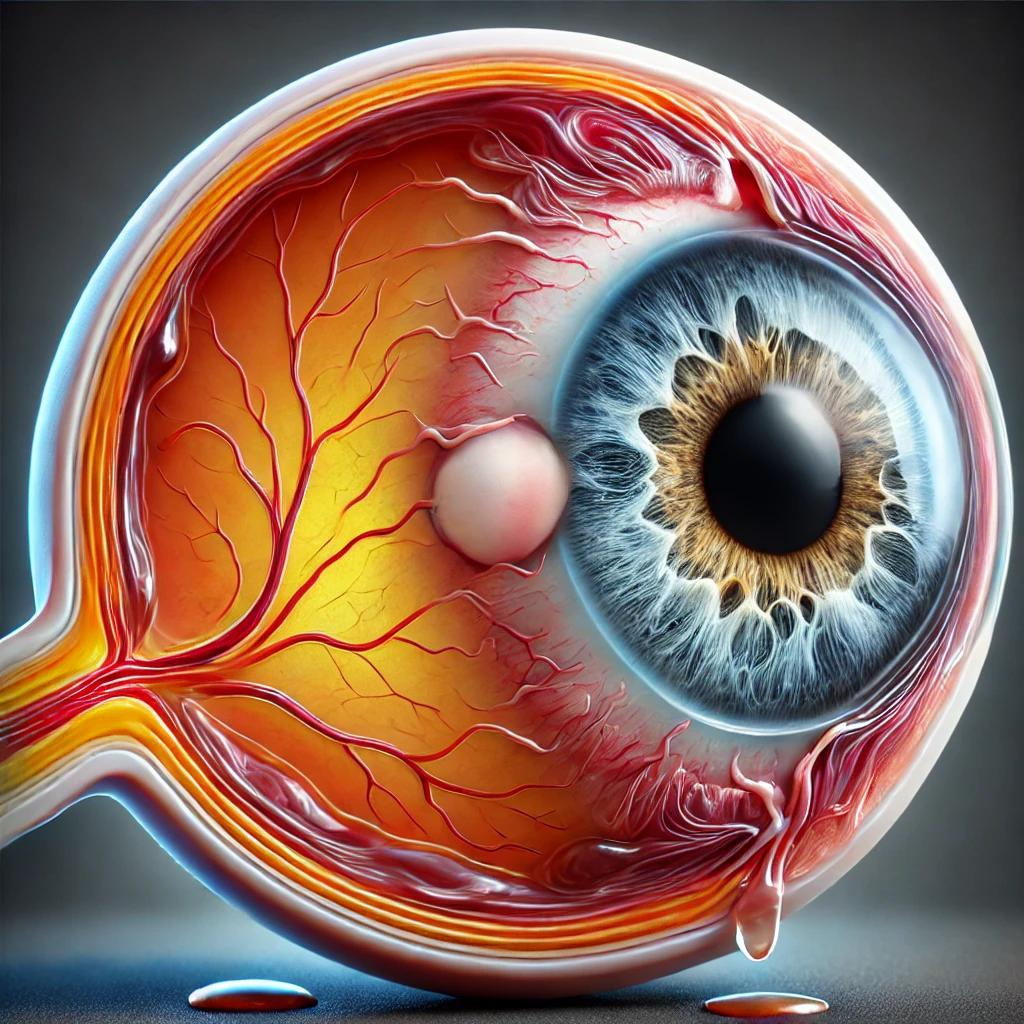
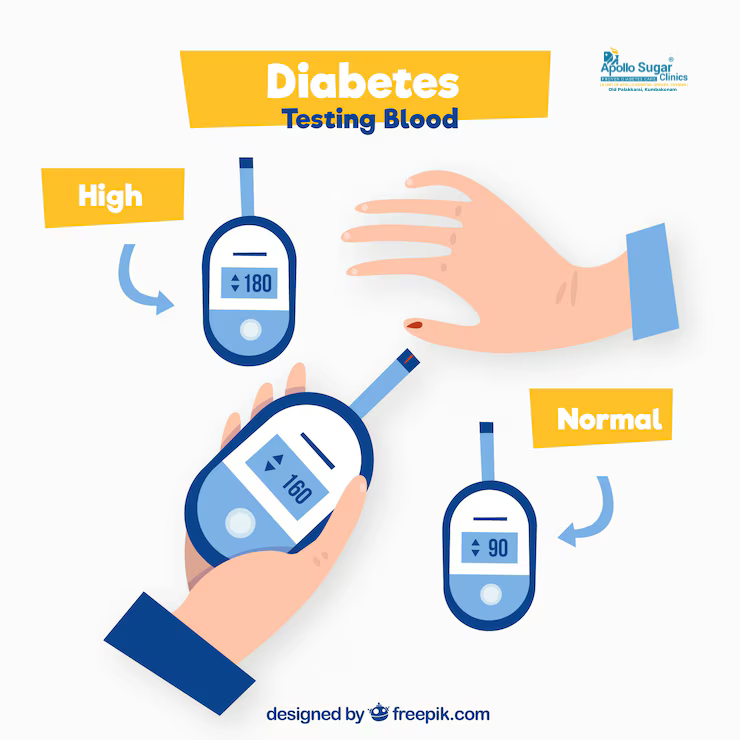
Diabetes Management Kumbakonam Comprehensive Diabetes Management and Care in Kumbakonam: Your Path to Better Health Introduction Are you or a loved one dealing with diabetes in Kumbakonam? Managing diabetes is crucial for maintaining your overall health and well-being. At Apollo Sugar Clinics, we specialize in providing comprehensive care and effective treatments for diabetes to help you live a healthy, balanced life. Understanding Diabetes What Is Diabetes? Diabetes occurs when your body is unable to properly regulate blood sugar (glucose) levels. It can cause various symptoms, including excessive thirst, frequent urination, fatigue, and blurred vision. Diabetes is commonly associated with obesity, poor diet, and sedentary lifestyles, but it can also be caused by genetic factors, autoimmune responses, or insulin resistance. Symptoms of Diabetes Increased Thirst: Excessive thirst, especially in the evening, is a common early sign of diabetes. Frequent Urination: Needing to urinate more often, especially at night, can indicate high blood sugar levels. Fatigue: Feeling unusually tired or weak can result from fluctuating blood sugar. Blurred Vision: Uncontrolled diabetes can affect your eyes, leading to blurred vision. Slow Healing of Wounds: Persistent sores or cuts that heal slowly can be a warning sign of diabetes. Diabetes Treatments Immediate Treatments If you experience symptoms of diabetes, immediate action is required to manage blood sugar levels. Here are some quick treatments: Insulin Therapy: For Type 1 diabetes or severe cases of Type 2, insulin injections help regulate blood sugar levels. Oral Medications: Drugs like metformin are commonly prescribed to lower blood sugar in Type 2 diabetes. Long-Term Management Long-term diabetes management involves understanding your condition and making necessary lifestyle adjustments: Dietary Changes: Adopt a balanced diet rich in whole grains, lean proteins, and vegetables while avoiding sugary and processed foods. Regular Exercise: Incorporate physical activity into your daily routine to improve insulin sensitivity and regulate glucose. Routine Monitoring: Regularly check your blood sugar levels to keep them within the recommended range. Stress Management: Chronic stress can impact blood sugar levels, so finding ways to manage stress is essential. Our Approach to Diabetes Treatment in Kumbakonam Comprehensive Assessment During your initial visit, our experienced healthcare professionals will conduct a thorough assessment to understand your medical history, current health status, and specific needs. This may include blood tests, HbA1c evaluations, and screenings for potential diabetes complications. Personalized Treatment Plan Based on your assessment, we will develop a personalized treatment plan tailored to your unique needs. This plan may include a combination of medications, lifestyle recommendations, and regular monitoring to help you maintain stable blood sugar levels. Ongoing Support and Monitoring We provide continuous support and monitoring to ensure your treatment plan is effective. Regular follow-up appointments and consultations help us track your progress, make necessary adjustments, and offer guidance to manage your diabetes effectively. Why Choose Us? Expertise and Experience: Our team of skilled healthcare professionals specializes in diabetes management, ensuring you receive the best care possible. Patient-Centered Care: Your comfort and well-being are our top priorities. We strive to provide personalized care that addresses your specific needs and concerns. Advanced Technology: We use the latest medical technology and equipment to provide accurate diagnoses and effective treatments. Comprehensive Services: In addition to diabetes treatment, we offer a wide range of services to support your overall health, including dietary counseling and foot care. BOOK YOUR APPOINTMENT TODAY! If you or a loved one is experiencing symptoms of diabetes, schedule a consultation with us at our Kumbakonam location. Our friendly and knowledgeable staff is here to help you achieve stable blood sugar levels and improve your quality of life. F.A.Q 1. What are the common symptoms of diabetes? Common symptoms of diabetes include: Increased thirst and frequent urination Fatigue Blurred vision Unexplained weight loss Slow healing of cuts or wounds If you experience these symptoms, it’s important to get your blood sugar levels tested. 2. What services do you offer for diabetes management at Apollo Sugar Clinics in Kumbakonam? We offer comprehensive diabetes care including: Blood glucose monitoring Personalized treatment plans Insulin therapy and medication management Nutritional and lifestyle counseling Regular health check-ups and screenings for diabetes complications 3. How often should I check my blood sugar levels? The frequency of blood sugar monitoring depends on your diabetes type and treatment plan. For Type 1 diabetes, daily monitoring may be necessary, while Type 2 diabetes patients may need to check a few times a week or as recommended by their doctor. 4. What is HbA1c, and why is it important? HbA1c is a blood test that shows your average blood sugar levels over the past 2-3 months. It’s a crucial test for determining how well your diabetes is managed. Keeping your HbA1c within a target range helps reduce the risk of complications. 5. Can diabetes be reversed? Type 2 diabetes can often be managed or even reversed with lifestyle changes such as a healthy diet, regular exercise, and weight loss. However, Type 1 diabetes is a lifelong condition that requires ongoing insulin therapy. 6. What dietary changes are recommended for managing diabetes? A balanced diet is essential for managing diabetes. We recommend: Focusing on whole grains, lean proteins, and vegetables Avoiding sugary snacks and beverages Eating smaller, frequent meals to maintain stable blood sugar levels Our dietitians at Apollo Sugar Clinics provide personalized meal plans to help you manage your diabetes effectively.